- Home
- A Race Against Time: Accelerating the Adoption of GDMT in Heart Failure
A Race Against Time: Accelerating the Adoption of GDMT in Heart Failure
- Heart Failure
Available Credit:
- Not accredited
Course Published On:
Course Expiry Date:

Overview
This symposium emphasises the critical role of accurate and rapid diagnosis in enabling physicians to quickly start guideline-directed medical therapy. Prof Antoni Bayes-Genis (University Hospital Germans Trias i Pujol, Barcelona, ES), Dr Lisa Anderson (St George's Hospital, London, UK) and Dr Stephen Greene (Duke University School of Medicine, Durham, US) discuss and reflect on current guidelines and emerging algorithms, offering insights into the challenges surrounding delays and adoption rates in both community and hospital settings and their profound impact on patient care.
Presented, and recorded, at HFA 2024 in Lisbon, PT
Support Statement
This Satellite Symposium was supported by an unrestricted educational grant from AstraZeneca who had no involvement in the content.
Target Audience
- Cardiologists
- Heart Failure Specialists
Learning Objectives
Upon completion of this activity, participants will be able to:
- Recall guideline recommendations for the use of NT-proBNP in heart failure
- Describe current practices in heart failure diagnosis and the impact on treatment outcomes
- Develop an optimised approach to the timely diagnosis and management of heart failure
Module |
Title |
Duration |
Speakers |
|---|---|---|---|
| 1 | Welcome and Introduction | 4m 44s | Lisa Anderson |
| 2 | Implementing GDMT: What Should We Be Doing? | 15m 59s | Antoni Bayés-Genís |
| 3 | Implementing GDMT: What Is Really Happening? | 17m 13s | Lisa Anderson |
| 4 | The Implication of Delayed Diagnosis and Sub-Optimal GDMT | 14m 13s | Stephen J Greene |
| 5 | Panel Discussion & Audience Q&A - Accelerating the Adoption Of GDMT | 2m 32s | Antoni Bayés-Genís |
| 6 | Key Take-Home Messages and Close | 43s | Antoni Bayés-Genís |
The Implication of Delayed Diagnosis and Sub-Optimal GDMT
Duration: 14m 13s
Speakers: Stephen J Greene
Panel Discussion & Audience Q&A - Accelerating the Adoption Of GDMT
Duration: 2m 32s
Speakers: Antoni Bayés-Genís
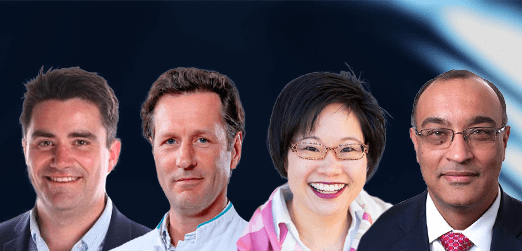
Chair
Speaker